H&p Coding Guidelines
Recovery Audit Contractors will likely continue to target high level initial hospital encounters for improper payments. The 1995 and 1997 EM documentation guidelines no longer apply.

H P Assessment Note Writing Outpatient Visits New Patients Minutes 3 Components Problem Focused History Problem Focused Exam Straightforward Ppt Download
The handbook also offers details on how to deter-mine critical care in order to choose the most accurate code.
H&p coding guidelines. Billing and Coding Guidelines. Report CPT codes 11102-11107 only for diagnostic biopsies and do not bill these codes with a screening diagnosis code. The regulation does not exempt ASCs that perform less invasive procedures from the requirement for a.
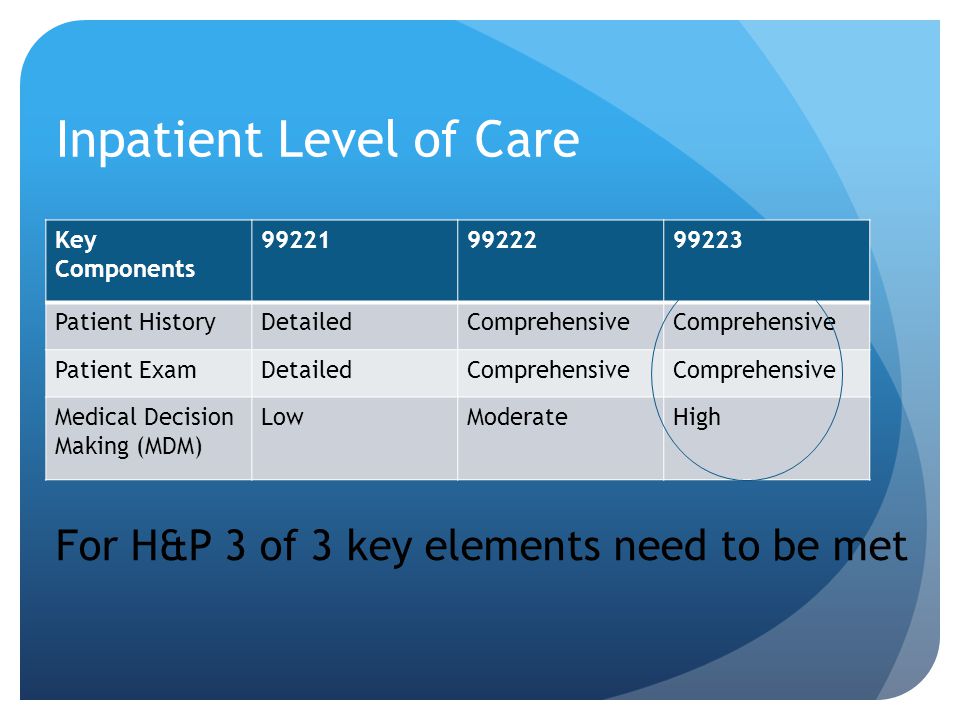
Acute inpatient care is reimbursed under a diagnosis-related groups DRGs system. Modifier 57 Decision for Surgery is appended to the EM code to indicate this is the decision-making service not the history and physical HP alone. The hospitalist will bill another initial hospital code 9922199223 based on what was performed and documented.
The orthopedic surgeon will bill for the initial hospital care 9922199223 and use modifier AI to indicate he is the principal physician of record. Before a condition can be coded it must meet two requirements. Coding chronic conditions only applies to inpatient not outpatient.
Medicare requires history and physicals HP for outpatient-based procedures and they must not be performed more than 30 days prior to the date of any scheduled surgical procedure regardless of the type of procedure Title 42 Part 41652a1 of the Code of Federal Regulations. Select the code based on the total floorunit time and bedside time. These guidelines should be used as a companion document to the official version of the ICD-10-.
This is the most popular code used to bill for admission HPs among internists who selected the 99223 level of care for 6773 of these encounters in 2018. Select the code based on the total face to face time spent by the attending physician with the patient for the entire visit Inpatient setting. The correct inpatient consultation codes for a first evaluation are 99221-99223.
CPT Surgery Coding Guidelines AHIMA 2008 Audio Seminar Series 6 NotesCommentsQuestions Surgical Documentation Guidelines Accurate and complete coding should paint a picture of the patients encounter Only documented services may be coded The physician documentation is key to correct code assignment and appropriate reimbursement. These codes are used for the inpatient History and Physical H P as well as any specialty consultation limited to one visit from each specialty. Every record has to stand on its own individual merits.
The HP should specifically indicate that the patient is cleared for surgery in an ambulatory setting. An H P must be completed and entered into the medical record for any high-risk procedure surgical procedure and any procedure that involves anesthesia services. 1 Uncertain Diagnosis If the diagnosis documented at the time of discharge is qualified as probable suspected likely questionable possible or still to be.
If the decision for surgery occurs the day of or before the major procedure and includes the preoperative evaluation and management EM services then this visit is separately reportable. Coding can be based on MDM or time with new times for each EM code. One the condition has to be documented by a physician in the body of the medical record such as history and physical consultant report progress notes or discharge summary.
This lecture will assist physicians and other non-physician practitioners NPPs determine if their initial hospital admission note documentation meets criteria for a level 2 mid level HP or a level 3 high level HP evaluation and management EM code. 19951997 EM documentation guidelines have been replaced by medical decision-making MDM or total time for office visit EM codes. DRGs are classifications of diagnoses and procedures in which patients demonstrate similar resource consumption and length-of-stay patterns.
Documentation Requirements Outpatient setting. The HP must be completed and documented for each ASC patient no more than 30 calendar days prior to date the patient is scheduled for surgery in the ASC. Coding guidelines for reporting chronic conditions is not superseded by whether or not there is a HCC vs a non-HCC and just to.
In cases where the patient is scheduled for two surgeries in the ASC within a short period. History and exam elements are no longer required for code selection. All elements times and content must be documented by the attending.
And Human Services DHHS provide the following guidelines for coding and reporting using the International Classification of Diseases th Revision Clinical Modification ICD-10-10CM. Qualified Practitioners The H P must be completed and documented by a qualified and privileged physician or other qualified licensed practitioner privileged to do so in accordance. This easy-to-use handbook includes an explanation of evaluation and management codes for the ED and how to deal with the challenges of undercoding.
Modifier 59 distinct procedural service should be appended to the biopsy code if applicable. Likewise the term HP is a hospital term not a coding term. The 30-day requirement mentioned above is typically a hospital requirement not a coding guideline.
Level 3 Admission HP 99223 The 99223 represents the highest level of initial care for patients being admitted to the hospital. A payment rate is set for each DRG and the hospitals Medicare. The guidance in the article referring to the 2007 CC re.
An HP is a hospital requirement not a billable service. These guidelines should be used as a companion document to the official version of the ICD-10-. In the past the codes 99221-99223 were used only for the admitting physicians and the codes 99251-99255 were designated for consulting physicians.
The new guidelines do not apply to any other EM services such as hospital emergency room or nursing facility codes. And Human Services DHHS provide the following guidelines for coding and r eporting using the International Classification of Diseases th Revision Clinical Modification ICD-1010-CM. Physicians do not get paid for doing dictation.
CPT codes and guidelines in order to report procedures accurately. The ICD-9-CM Official Guidelines for Coding and Reporting Sections IIH and IIIC state. Code 99201 has been removed as the MDM was the same as 99202.
Check National Correct Coding Initiative NCCI edits. Apply the appropriate modifier to the appropriate code.

Coding And Documentation Made Easier Fpm

Get Ready For 2021 Coding Changes Part 2 Gutsandgrowth
Level 3 H P 99223 E M Coding Education Em Evaluation And Management Coding E M Documentation 99214 99213

Coding And Documentation Made Easier Fpm

Coding And Documentation Made Easier Fpm
Hospitalist Coding And Billing For Dummies Ppt Video Online Download

Posting Komentar untuk "H&p Coding Guidelines"